|
Ankle sprains are a common but painful injury that can temporarily limit your mobility. Recent studies have shed light on the most effective treatments for managing this condition. A systematic umbrella review by Gaddi et al. (2022) in Frontiers in Medicine examined multiple studies to establish a clear guide for treating acute ankle sprains. Here’s what you need to know to navigate the recovery from an ankle sprain effectively.
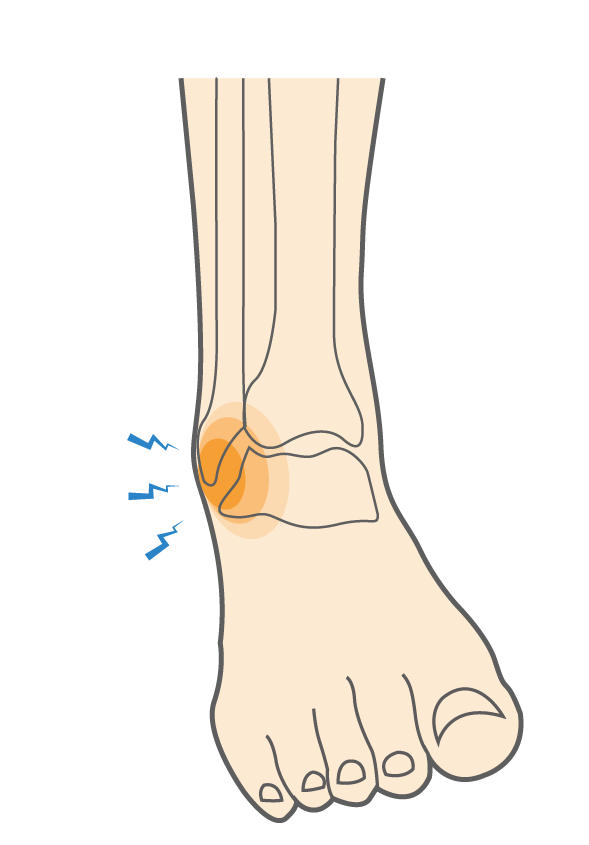
Understanding Ankle SprainsAnkle sprains occur when the ligaments that stabilise the ankle are overstretched or torn, usually due to twisting or rolling the foot. Symptoms typically include pain, swelling, and limited mobility. While these injuries are prevalent, especially in physically active individuals, understanding the latest research can significantly aid recovery. Effective Non-Surgical TreatmentAccording to Gaddi et al. (2022), non-surgical interventions are highly effective in managing acute ankle sprains. These treatments focus on minimising pain and swelling while optimising the healing process without the need for surgery. Here are the key findings:
ConclusionRecovering from an ankle sprain requires patience and adherence to proven treatment protocols. The insights from the umbrella review by Gaddi et al. (2022) emphasise the importance of functional recovery programs and appropriate pain management, tailored to individual needs and medical advice. By following these evidence-based recommendations, patients can expect a more efficient and effective recovery. References
0 Comments
In the quest for muscle strength, hypertrophy, and endurance, the principle of progressive overload stands as a cornerstone of resistance training. Traditionally, increasing the weight (load) you lift has been the go-to method for achieving this. However, recent research sheds light on an equally effective strategy that might just change the way we approach our workouts: increasing repetitions while maintaining the same load. Let's dive into what this means for your training regimen.
Understanding Progressive Overload Progressive overload involves gradually increasing the demands on your musculoskeletal system, thereby stimulating muscle growth, strength, and endurance. Traditionally, this has meant adding more weight to the bar. However, is this the only way to achieve muscular adaptations? The Study: Load Increase vs. Repetition Increase A groundbreaking study published in PeerJ (2022) by Plotkin et al. compared two groups over an 8-week period to see which method of progressive overload was more effective: increasing load or increasing repetitions[1]. Participants, all of whom had at least one year of lower body resistance training experience, were divided into two groups:
Key Findings The study found that both methods led to muscular adaptations, with some interesting nuances:
Implications for Training These findings offer valuable insights for trainers and trainees alike, presenting another promising approach to programming resistance training. Here's what it means for your workouts: Flexibility in Training The study underscores the viability of both increasing loads and increasing repetitions for enhancing muscular adaptations. This flexibility allows for personalised training programs that can be adjusted based on individual goals, preferences, and the availability of equipment. Tailored Goals
For individuals recovering from injuries or those concerned about the risk of overloading with heavy weights, increasing repetitions offers a safer yet effective method of achieving progressive overload without the need to constantly increase the weight lifted. Conclusion The study by Plotkin et al. illuminates a path forward for those looking to optimise their resistance training strategy, offering evidence that both increasing loads and repetitions can lead to significant muscular adaptations. Whether your goal is muscle growth, strength, endurance, or rehabilitation, incorporating a mix of both strategies into your workout regimen can provide comprehensive benefits tailored to your unique fitness journey. Embrace the flexibility in your training approach, and remember, the best workout is the one that is personalised, progressive, and most importantly, enjoyable! Reference
When embarking on a resistance training journey, one of the most common dilemmas faced by beginners and seasoned gym-goers alike is choosing between multi-joint (MJ) and single-joint (SJ) exercises. Both types of exercises offer unique benefits and can be pivotal in shaping your fitness regimen. Recent studies shed light on their effects, helping you make an informed decision tailored to your goals.
Understanding the Basics Multi-Joint Exercises involve two or more sets of joints and muscle groups. Classic examples include squats, bench presses, and deadlifts. These exercises are lauded for their efficiency in working multiple muscles simultaneously, potentially offering greater functional benefits. Single-Joint Exercises focus on isolating one joint and primarily targeting a single muscle group, like bicep curls or leg extensions. They are often recommended for targeted muscle development and rehabilitation purposes. The Research SpeaksTwo significant studies provide insight into the ongoing debate between MJ and SJ exercises. Gentil et al. (2015) found that both MJ and SJ exercises produced similar increases in muscle size and strength in untrained men, suggesting that neither type is superior for beginners aiming to increase muscle mass and strength[1]. On the other hand, Paoli et al. (2017) demonstrated that when the total work volume was equated, MJ exercises led to greater improvements in VO2max and muscle strength than SJ exercises[2]. This suggests that MJ exercises might offer added benefits for improving cardiovascular fitness and functional strength. Making the Choice: What's Best for You? The selection between MJ and SJ exercises should align with your fitness goals, practical considerations, and personal preferences:
Both MJ and SJ exercises have their place in a well-rounded fitness regimen. Understanding your personal goals, whether it's muscle gain, fat loss, strength, rehabilitation, or general fitness, is key to determining the right balance between the two. Consultation with fitness and health professionals can provide personalized advice and training programs, ensuring you get the most out of your workouts while minimizing the risk of injury. Remember, the best exercise program is one that is sustainable, enjoyable, and tailored to your individual needs and goals. So, whether you're lifting heavy with the squats or focusing on that bicep peak with curls, you're on the right track to achieving your fitness aspirations. References
The deadlift, often perceived as an exercise reserved for the most robust and athletic individuals, holds a treasure trove of benefits that extend well beyond the realms of elite sports. This fundamental movement not only enhances strength and performance but also plays a pivotal role in the rehabilitation and maintenance of back health for people of all ages. Through a careful examination of recent research, we unveil the multifaceted benefits of deadlifts and debunk the myth that they are unsafe for individuals with lower back pain.
Unveiling the Benefits Deadlifts are more than just a strength-building exercise; they are a functional movement that mimics everyday activities such as lifting heavy objects off the ground. This exercise targets multiple muscle groups, including the glutes, hamstrings, lower back, and core, providing a comprehensive workout that can improve overall physical health and functionality. Research indicates that incorporating deadlifts into a training program can result in significant improvements in lower body strength and power. A study comparing the effects of deadlifts and squats found that both exercises led to comparable enhancements in jump performance, a marker of lower body power (Nigro & Bartolomei, 2020)[1]. Moreover, deadlifts have been shown to have the highest muscle activation of paraspinal musculature compared to other exercises, making them a potent tool for strengthening the muscles supporting the spine (Fischer, Calley, & Hollman, 2020)[2]. Safety and Efficacy for Lower Back Pain The prevalence of lower back pain in the general population has led to significant interest in finding effective exercises for both rehabilitation and prevention. Contrary to common misconceptions, deadlifts, when performed with proper technique, can be a safe and effective exercise for individuals with lower back pain. A systematic review highlights that exercise programs including deadlifts can yield improvements in both pain and function for those living with low back pain, although not more beneficial than low load motor control exercises (Fischer et al., 2020)[2]. It is crucial, however, to note that individuals with lower pain levels and higher baseline lumbar extension strength may be most suitable for deadlift programs. This finding underscores the importance of personalised assessment and program design by healthcare professionals. Implementing Deadlifts into Your Routine For those considering adding deadlifts to their exercise regimen, especially individuals with a history of lower back pain, consulting with a physiotherapist is essential. These experts can assess your current physical condition, teach proper deadlift technique, and develop a tailored program that aligns with your health goals and capabilities. It is also worth noting that starting with lighter weights and focusing on form over load can significantly reduce the risk of injury and ensure the long-term success of incorporating deadlifts into your routine. Conclusion The deadlift is a versatile exercise that offers extensive health and performance benefits for individuals across all age groups. Its efficacy in strengthening the lower back, improving functional performance, and aiding in the rehabilitation of back pain makes it a valuable addition to any exercise program. With proper guidance and technique, deadlifts can be safely performed by people with varying levels of fitness, including those with lower back pain, debunking the myth that they are inherently risky. By embracing the deadlift, individuals can enjoy a healthier, more active lifestyle, underscored by the strength and stability this foundational movement provides. References
Anterior Cruciate Ligament (ACL) injuries are a common concern among athletes and physically active individuals, often leading to a challenging decision: to opt for surgery or explore non-surgical treatment options. Recent research provides compelling evidence that ACL ruptures can potentially heal on their own, offering an alternative pathway to recovery without the need for surgical intervention. This blog post delves into the findings of two significant studies that shed light on the natural healing capabilities of the ACL and the implications for treatment strategies.
Healing of ACL Ruptures: Insights from the Cross Bracing Protocol Study A groundbreaking study published in the British Journal of Sports Medicine by Filbay et al. (2023) investigated the outcomes of non-surgical management of acute ACL ruptures using the Cross Bracing Protocol (CBP). This protocol entails knee immobilisation at 90° flexion in a brace for four weeks, followed by progressive increases in range-of-motion until brace removal at 12 weeks, and physiotherapist-supervised, goal-oriented rehabilitation. The study's findings are encouraging, showing that 90% of patients had evidence of ACL healing on a 3-month MRI. Participants with better healing outcomes reported higher scores on the Lysholm Scale and ACL Quality of Life (ACLQOL), experienced normal knee laxity, and were more likely to return to pre-injury levels of sport participation. These results highlight the potential of non-surgical management to support ACL healing, suggesting that such approaches could lead to favourable outcomes for certain patients. The KANON Trial: A Secondary Analysis on ACL Healing and Patient-Reported Outcomes Further supporting the potential for non-surgical recovery, a secondary analysis from the KANON trial, also published in the British Journal of Sports Medicine by Filbay et al. (2023), evaluated the natural course of ACL healing and its association with patient-reported outcomes. This analysis focused on participants who were managed with rehabilitation alone, comparing their outcomes to those who underwent early or optional delayed ACL reconstruction. The results revealed that 53% of participants managed with rehabilitation alone exhibited MRI evidence of ACL healing at the 2-year follow-up. These individuals reported significantly better outcomes in terms of sports and recreational function, as well as quality of life, compared to those without evidence of healing or who underwent ACL reconstruction. The findings suggest that a considerable proportion of adults with ACL ruptures could achieve spontaneous healing, leading to favourable clinical outcomes. Implications for Treatment Strategies These studies challenge the conventional wisdom that surgery is the only solution for ACL ruptures, opening the door to non-surgical treatment options for selected patients. The evidence points towards the natural healing capabilities of the ACL, suggesting that with appropriate management, including bracing and physiotherapy-led rehabilitation, patients can achieve successful outcomes without the need for surgical intervention. It is essential to recognise that the decision between surgical and non-surgical treatment should be personalised, taking into account the individual's specific circumstances, injury characteristics, and lifestyle needs. Patients should consult with healthcare professionals, including physiotherapists, to determine the most suitable treatment pathway for their situation. Conclusion The potential for ACL ruptures to heal without surgery offers a promising alternative for patients seeking non-surgical treatment options. The findings from recent research underscore the importance of exploring all available treatment pathways and highlight the role of physiotherapy in supporting recovery from ACL injuries. As we continue to learn more about the ACL's natural healing process, it is crucial to keep an open mind regarding the best practices for managing these challenging injuries. References
In the realm of orthopaedic injuries, meniscal tears stand out as both common and challenging, particularly in active individuals. Traditionally, arthroscopic partial meniscectomy (APM) has been a go-to treatment for these injuries, aiming to relieve pain and restore function. However, recent research suggests a pivotal shift in our approach—highlighting the effectiveness of conservative management, including physical therapy, over arthroscopy for certain cases. This blog post explores the evidence from recent studies, advocating for a more measured approach to treating partial meniscal tears.
The Debate: Arthroscopy vs. Physiotherapy A landmark study published in the British Journal of Sports Medicine by van der Graaff et al. (2023) compared outcomes between arthroscopic partial meniscectomy and physical therapy in young patients with traumatic meniscal tears. This randomised controlled trial found no significant difference in International Knee Documentation Committee (IKDC) scores, which measure symptoms, knee function, and sports activity levels, at 24 months follow-up between the two groups. Interestingly, 41% of patients initially managed with physical therapy did not require subsequent arthroscopy, challenging the necessity of immediate surgical intervention. Broadening the Perspective: Systematic Reviews Further backing this shift, a systematic review by Brignardello-Petersen et al. (2017), published in BMJ Open, examined the effects and complications of knee arthroscopy compared with conservative management in patients with degenerative knee disease. The review found high-certainty evidence that knee arthroscopy offers very small to no long-term benefits in pain or function over conservative strategies. Similarly, Rotini et al. (2023) conducted a systematic review of systematic reviews, which concluded that exercise therapy often equals or surpasses arthroscopic surgery in improving pain and function for degenerative meniscal lesions. Implications for Clinical Practice These findings underscore a critical reassessment of the routine use of arthroscopy for partial meniscal tears, particularly in the context of degenerative knee conditions. Physiotherapy, focusing on strengthening and stabilising the knee joint, emerges as a potent first-line treatment option that can defer or even eliminate the need for surgery in many cases. However, it's essential to acknowledge that surgical intervention may still be necessary for specific patient populations. The challenge lies in accurately identifying those who may benefit from surgery after an unsuccessful trial of conservative treatment. Conclusion The shift towards conservative management for partial meniscal tears represents a more patient-centric approach, minimising the risks and costs associated with unnecessary surgery. These recent studies provide compelling evidence that physical therapy should be considered the first line of treatment for many patients with meniscal tears. As we move forward, personalised treatment plans, grounded in the latest research and tailored to each patient's unique situation, will likely yield the best outcomes. References
Subacromial bursitis, a common source of shoulder pain, often leads patients and healthcare providers to consider arthroscopic interventions. However, recent studies advocate for a more conservative approach, emphasising physiotherapy interventions that challenge the necessity of surgery. This blog post delves into the effectiveness of non-surgical treatments for subacromial bursitis, highlighting key findings from recent research that support exercise therapy and manual therapy as first-line treatments.
The Role of Exercise Therapy in Managing Subacromial Bursitis A systematic review published in the Journal of Orthopaedic & Sports Physical Therapy (2020) by Louise Pieters and colleagues, underscores the significant benefit of exercise therapy for patients with subacromial shoulder pain (1). The review, which updated a previous 2013 examination, strongly recommends exercise therapy as the initial treatment strategy to improve pain, mobility, and function. It further suggests that manual therapy could be effectively integrated as an adjunct to exercise, providing a holistic approach to treatment. Interestingly, the review found moderate evidence indicating that other commonly prescribed interventions, such as laser therapy, extracorporeal shockwave therapy, and ultrasound, had no significant effect. Proprioceptive-Based Strategies: A New Frontier The exploration of proprioceptive-based strategies for treating subacromial impingement syndrome offers a refreshing perspective on managing shoulder pain. A systematic review by Harman Singh, Aaronvir Thind, and Nequesha S Mohamed, published in Cureus (2022), evaluated the effectiveness of kinesiology tape, myofascial trigger point release (MPTR), scapular stabilisation exercises (SSE), and resistance training compared to traditional modalities (2). Their findings reveal that all examined techniques demonstrated some degree of effectiveness in reducing pain and improving function, although the evidence suggests a need for further large-scale studies to solidify these outcomes. Understanding the Clinical Course of Subacromial Shoulder Pain A systematic review with meta-analysis conducted by Zohreh Jafarian Tangrood and colleagues, published in 2023, sought to understand the clinical course of pain and function in patients with subacromial pain (3). The study's insights are invaluable, revealing that without intervention, minimal improvement can be expected within the first three months. Conversely, 'usual care' - encompassing a broad range of conservative treatments - showed significant improvement in pain and function up to 12 months, with a substantial portion of this improvement occurring in the first six weeks. The Effectiveness of Physiotherapy Exercises The evidence supporting physiotherapy exercises for subacromial impingement syndrome continues to grow, as highlighted in a systematic review and meta-analysis by Hanratty CE and colleagues (4). This comprehensive analysis reinforces the notion that individually tailored physiotherapy exercises can lead to significant improvements in pain and function, further challenging the immediate recourse to surgical interventions. ConclusionThe shift towards conservative management of subacromial bursitis, particularly through exercise therapy and manual therapy, is backed by a growing body of research. These studies collectively underscore the potential for significant improvements in pain, function, and mobility without the need for surgical intervention. As the healthcare community continues to advocate for evidence-based practices, the emphasis on physical therapy interventions as a first-line treatment offers a promising avenue for patients struggling with subacromial bursitis, advocating for a less invasive, more holistic approach to care. References
In the competitive world of sports and the meticulous field of physiotherapy, discussions frequently orbit training methodologies, nutritional strategies, and the forefront of recovery technologies. However, a crucial element in athletes' well-being and recuperation that is often overlooked is the role of sleep. Emerging research unequivocally emphasises the profound impact of sleep on injury recovery and athletic performance, spotlighting its indispensable role in an athlete's regimen. The Foundation of Recovery Sleep stands as a fundamental pillar in the body's recovery mechanism, providing not only rest but also facilitating cellular repair and hormonal equilibrium. A systematic review in the British Journal of Sports Medicine delineates the significant role of sleep in the convalescence of sports injuries, pointing out that inadequate sleep quality and duration are common among athletes and considerably amplify injury risks . This body of work stresses the importance of incorporating sleep management into training and competition schedules to curtail injury rates and expedite rehabilitation. Enhancing Muscle Recovery The intricate nexus between sleep and muscle recuperation is especially noteworthy. According to a narrative review in the Journal of Science and Medicine in Sport, extending sleep duration not only bolsters performance but also enhances pain sensitivity and anabolic responses, such as elevated levels of GH/IGF-I, pivotal for muscle repair and recuperation from exercise-induced injuries. This evidence suggests that sleep interventions could serve as a critical tool in hastening recovery processes, presenting a topic of keen interest for medical professionals and coaches alike. Sleep’s Role in Injury Risk Management Further research detailed in the Journal of Sports Rehabilitation elucidates the association between sleep and injury risk, demonstrating that chronic insufficient sleep is correlated with an increased risk of musculoskeletal pain and sports injuries. Specifically, consistently sleeping less than seven hours is linked with a higher injury risk, underscoring the necessity of adequate sleep for injury prevention . The Impact on University Athletes The challenge of managing sleep extends beyond professional athletes to include university athletes as well. A study published in Frontiers in Sports and Active Living reveals how academic and social stresses can exacerbate sleep disruption, leading to adverse effects such as performance decline, mood alterations, and an increased vulnerability to injuries and illnesses. This highlights the widespread applicability of sleep management strategies across different levels of athletic engagement. Practical Implications for Your Recovery Journey For athletes embarking on the recovery path, or anyone aspiring to elevate their physical performance, the directive is clear: sleep must be prioritizsed. Here are actionable steps to integrate into your routine:
The expanding corpus of research on sleep's effects on injury recovery and athletic performance furnishes invaluable insights for athletes, coaches, and healthcare practitioners. As we delve deeper into the myriad benefits of sleep, it becomes increasingly clear that sleep is not merely a passive rest period but a dynamic process integral to athletes' health, well-being, and achievement. By prioritising sleep, we can optimise our recovery processes, mitigate injury risks, and unlock our utmost potential in sports and beyond References Used
Most of us are aware that physical activity is widely recognised as a key factor in promoting health and longevity. But how does engaging in sports specifically contribute to a longer life? Recent studies shed light on the fascinating connection between sports participation and an increase in life expectancy. The Impact of Elite Sports on Longevity A groundbreaking report from the International Longevity Centre UK (ILC), funded by Bayes Business School, delves into the lives of Commonwealth Games competitors, revealing that top-level athletes live significantly longer than the general population. The study, titled “Marathon or sprint: Do elite-level athletes live longer than average?”, found that elite athletes enjoy a lifespan boost of up to 29% in certain sports compared to their contemporaries. This increase translates to an impressive 4.5 to 5.3 extra years of life for men and 3.9 years for women across various sports disciplines. The Surprising Link Between Social Sports and Longevity Exercise, in general, is key to living a longer life, but playing certain sports can further increase your life expectancy. According to the Copenhagen City Heart Study (CCHS) and findings published in the Mayo Clinic Proceedings, participation in specific sports leads to notable life expectancy gains. The study followed 8,577 people over 25 years, revealing significant longevity benefits associated with several sports:
Alpine skiing and cross-country skiing emerge as notable sports for promoting health and longevity. Alpine skiing is associated with higher values of health-related quality of life (HRQoL), physical self-concept (PSC), and intrinsic motivation among physically active older adults. Similarly, a population-based follow-up study highlights the benefits of cross-country skiing, showing it is associated with lower all-cause mortality. The Broad Benefits of Physical Activity Regular exercise reduces major mortality risk factors and increases life expectancy by 0.4 to 6.9 years for active individuals compared to those who are inactive. Encouraging Physical Activity for Everyone These studies highlight the profound impact of physical activity and sports participation on longevity. Whether it's through professional sports, leisure activities, or incorporating regular physical exercise into your routine, the benefits are significant. Tips for Getting Started and Sustaining Physical Activity
For our clients at Acland Street Physiotherapy, embracing physical activity is not just about enhancing immediate health outcomes but is a lifelong investment in your well-being. Our team is dedicated to supporting your active lifestyle, whether you're seeking rehabilitation, fitness improvement, or ways to extend your lifespan through exercise. Remember, it's never too late to start. Let the inspiring examples of athletes and the compelling findings from recent studies motivate you to integrate physical activity into your life, celebrating the joy of movement and the reward of extended health and longevity. References Used
In the quest for maintaining cognitive health as we age, the intertwining paths of physical strength and mental acuity offer an intriguing and promising avenue. Emerging research is shedding light on a powerful tool that goes beyond the conventional: strength training. Yes, the very practice often associated with muscle building and physical endurance also harbours profound benefits for our cognitive function. Here, we delve into the compelling evidence that underscores the mental enhancements brought forth by resistance training, particularly among older adults.
A Strong Body Houses a Sharp Mind A groundbreaking study by Matheus U Chupel and colleagues (2017) unveils that strength training diminishes inflammation while boosting cognition and physical fitness in older women with cognitive impairment. This research is pivotal in illustrating how resistance exercise fosters an anti-inflammatory balance, simultaneously uplifting physical performance and the cognitive profile. The implication? Engaging in strength training can be a strategic ally in combating cognitive decline, offering a beacon of hope for enhancing life quality in our golden years. The BDNF Connection: A Leap in Cognitive Health Diving deeper into the physiological underpinnings, a study by Emy S. Pereira et al. (2018) highlights the acute surge in Brain-Derived Neurotrophic Factor (BDNF) following a session of an extreme conditioning program. BDNF is no ordinary protein; it's central to brain health, implicated in learning, memory, and higher-order thinking. The study's findings suggest that not only does physical exercise stimulate this critical brain protein, but specific types of strength training can significantly elevate its levels, potentially unlocking immediate cognitive enhancements. Immediate and Lasting Cognitive Enhancements A systematic review by Jan Wilke et al. (2019) provides a broader perspective, affirming the immediate positive effects of resistance exercise on global cognition in healthy adults. This suggests that the benefits of lifting weights extend far beyond the physical realm, enhancing mental processes that are crucial for daily functioning and overall well-being. Strength Gains as Cognitive Gains Further substantiating the connection between physical and cognitive strength, a study led by Yorgi Mavros (2017) explores how strength gains from resistance training mediate improvements in cognitive function among older adults with mild cognitive impairment. This research underscores the significant role of muscle strength in enhancing cognitive function, advocating for strength training as a potent non-pharmacological intervention to fend off cognitive decline. Practical Insights for a Sharper Tomorrow Complementing these findings, André de Camargo Smolarek and colleagues (2016) observe that regular resistance exercises lead to noteworthy improvements in cognitive capacities of elderly women, emphasising enhanced life quality through strength training. Additionally, a systematic review by Zhihui Li et al. (2018) corroborates the efficacy of resistance training in bolstering executive cognitive abilities and global cognitive function, further advocating for its inclusion in the elderly's routine for a sharper mind. Starting Strength Training: Tips for Beginners Embracing strength training as a beginner might seem daunting, but it's a journey well worth embarking on for both your physical and cognitive health. Here are some tips to get you started:
Embracing Strength Training: A Path to Cognitive Resilience The evidence is compelling: integrating strength training into our exercise regimen can be a powerful strategy to preserve and enhance cognitive function, especially as we age. For physiotherapy practitioners and enthusiasts alike, these findings illuminate the profound impact of physical strength on mental health, advocating for a holistic approach to wellness that marries the vigor of the body with the vitality of the mind. As we continue to explore and understand the myriad ways in which exercise influences our cognitive landscape, it's clear that strength training holds a special place in the pantheon of tools at our disposal for combating cognitive decline and fostering a resilient, sharp mind throughout the lifespan. Incorporating strength training into our lives is more than a commitment to physical health; it's an investment in the longevity and vitality of our cognitive essence. For those embarking on this journey, the promise of a sharper, more vibrant mind awaits. References Used:
|
Author
Archives
May 2024
|
Copyright Acland Street Physiotherapy © 2024


 RSS Feed
RSS Feed