|
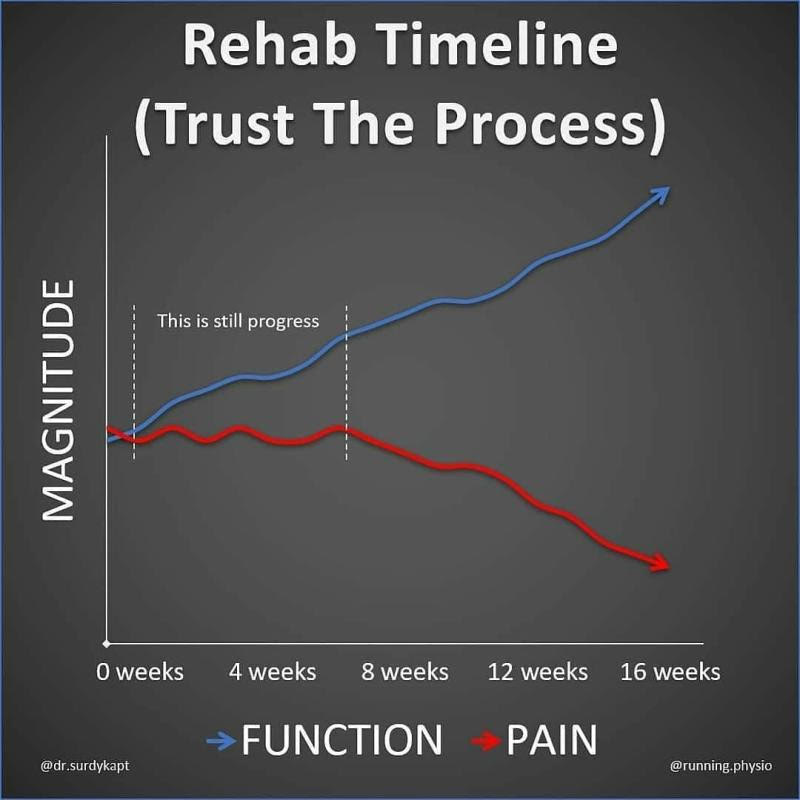
Patience and persistence are the keys to a successful physiotherapy rehabilitation program for your injury or following orthopaedic surgery. At Acland Street Physiotherapy, we try our best to set very realistic expectations of full recovery from the beginning of the physiotherapy treatment program. We have a relatively low patient drop out out rate to injury rehab programs that need to be committed to for at least 3 months. We enlighten and train our patients from the beginning of the physiotherapy treatment program that their movement or function will improve much before pain does. Realistically, pain will most probably come on for the journey but will reduce over time. Nonetheless, in some cases, pain may resolve with a rapid increase in function.
It is important to understand that for some people depending on the nature of the injury, the pain will resolve completely. For most people, pain will continue on at a relatively manageable level. They will experience a little bit of a niggle or discomfort now and then and this might be the "new normal" moving forward. The key point here is that be reassured with a comprehensive injury rehabilitation program, you will with time, be able to return to doing the things you love, and your pain will be relatively less in all cases. In addition, completely resting and avoiding activities is often not the answer and can lead to poorer results in the longer term.
6 Comments
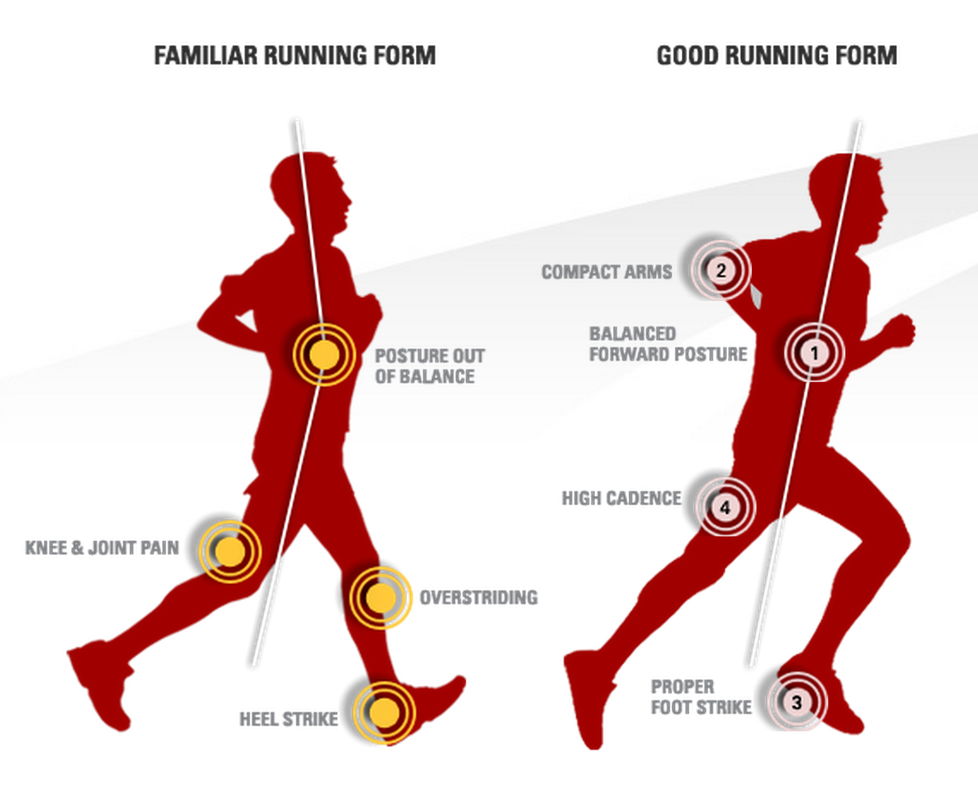
During the COVID-19 pandemic, running observably has become an extremely popular exercise activity locally obviously, for its health benefits and simplicity as no equipment is required. I am avid runner myself recreationally often clocking up 50kms per week. Over the past 10 years as a physiotherapist, I have coached hundreds of my patients who have never ran before to shed a few pounds or improve their overall fitness. Many of my patients have misconceptions about running in particular, that running is bad for your knees and that you are at major risk of arthritis. This common concern has been debunked by science by multiple studies. Based on large population studies, the chances of developing arthritis from regular running are very slim. In fact, regular running has shown to strengthen joints and plays a protective role in the development of osteoarthritis later in life. Commonly reported knee pain by runners at Acland Street Physiotherapy that is generally treatable with a moderate amount of physiotherapy and strength training are Iliotibial Band Syndrome or Patellofemoral Pain Syndrome.
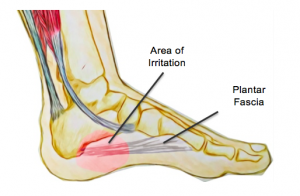
The following is a concise infographic on how what good running form generally looks like. If you would prefer to further explore this, please do not hesitate to make a booking with us for a comprehensive physiotherapy and biomechanical running assessment. Plantar fasciitis or "inner heel pain" can be a very painful condition that is the result of degeneration of the plantar fascia origin on the inside of the heel bone as well as the surrounding soft tissue supporting structures. The plantar fascia has a key role in providing arch support and shock absorption during weight bearing activities such as standing, walking and running.
It is often caused by an overuse or repetitive strain injury. Specifically, overuse causes micro-tears of the plantar fascia. Common risk factors include:
Before consider a cortisone injection, plantar fasciitis generally responds well to physiotherapy treatment including manual therapy, extracorporeal shockwave therapy, dry needling, stretches and specialised high load strengthening exercises. Lateral ankle sprains are very common among the active population and with proper professional guidance, can have serious long-term complications. Complications include fractures, recurrent sprains and ligamentous instability, resulting in surgery.
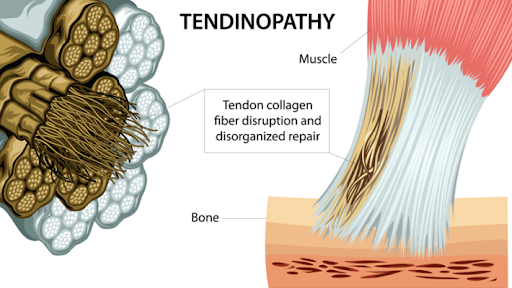
As a first point of call, it is important to get assessed by an experienced physiotherapist to get thoroughly assessed and diagnosed. Through history taking and physical examination, the physiotherapist will determine what ligaments have specifically been injured, the severity and whether an x-ray may be needed. Studies have shown that early mobilisation of a sprained ankle has significant benefits for improvements in pain, function and its long term stability. Physiotherapy treatment may include strategies to reduce swelling and inflammation, ankle taping/bracing, manual therapy to break up the scar tissue and an exercise rehabilitation program to help improve range of motion, strength, neuromuscular control and proprioception/balance. A high quality exercise rehabilitation program can get you back to what you were doing previously quickly and prevent injury recurrence. Tendinopathy is a generic term used to describe injuries to the tendon associated with inflammation and degeneration. It can be either characterised as a painful or pathological condition associated with overuse. Usually pain is associated with increased loads and a recognition that there has been a relative increase in inactivity. Pain is often reported as sharp early on and then becomes a dull ache weeks later. Pain may be present at the beginning of the activity then disappear during it, then returns on subsequent attempts of the activity.
Tendinopathies are common as they have a poor blood or nutrient supply compared to skeletal muscles. In fact, the oxygen consumption of tendons is about 7.5 times lower than skeletal muscles. A relatively low metabolic rate results in generally slow healing after injury. Common tendinopathies seen at Acland Street Physiotherapy include:
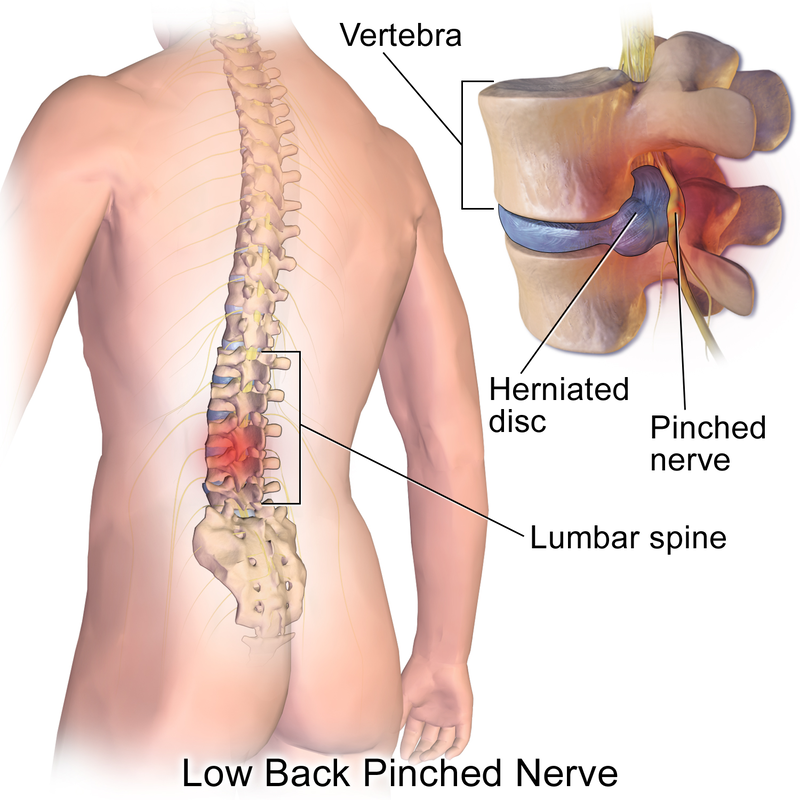
Tendinopathies generally respond well to physiotherapy treatment. This could include treatment techniques such as manual therapy, extracorporeal shockwave and eccentric strengthening exercises to improve the load capabilities of the tendon. One of the most common lower back complaints at Acland Street Physiotherapy is symptoms of a pinched nerve. This is a condition where lower back pain occurs as a result of a nerve in the lower spine is being compressed by a nearby bone or soft tissue structure. The pressure from the pinch may causes pain, numbness, burning or tingling in the lower back, legs or feet. Some people may also call this condition "sciatica".
The common causes of this condition are:
Often such conditions do not need further x-rays, CT scans or MRIs and respond extremely well to physiotherapy treatment, which may include manual therapy, heat therapy, dry needling, postural taping, pain and postural education and a specific exercise program. It is important to note that you should seek emergency medical attention or see your doctor if:
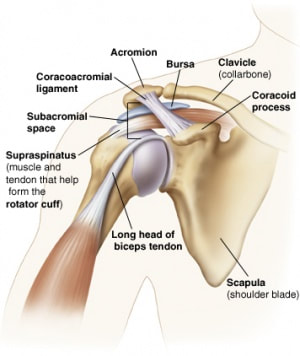
Frozen shoulder, "painful stiff shoulder" or "adhesive capsulitis" is characterised as an initially painful but progressive joint condition that causes limited range of motion over time. This is an inflammatory condition that causes fibrosis or "scarring" of the glenohumeral joint capsule. This condition is complex, often occurs in females, and is multifactorial involving both environmental and genetic factors. A major risk factor is diabetes type II. It can take 2-3 years to resolve and some patients may not ever fully recover. Treatment involves a combination of physiotherapy treatment (manual therapy and home exercises involving stretching, strengthening and mobilty) and medical management such as cortisone injections and hydrodilatations (distension arthrography). Subacromial pain syndrome is a non-traumatic one sided condition of the shoulder. This common condition is two thirds of all shoulder complaints at Acland Street Physiotherapy. This condition is more prevalent as you age. It usually causes pain localised around the acromion (bony process of the shoulder) when lifting the arm. Usually one or structures are injured within the subacromial space.
Common conditions that cause subacromial pain syndrome include:
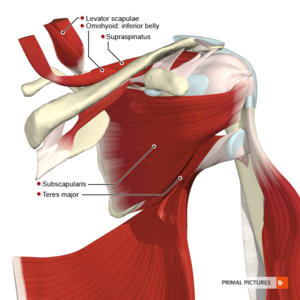
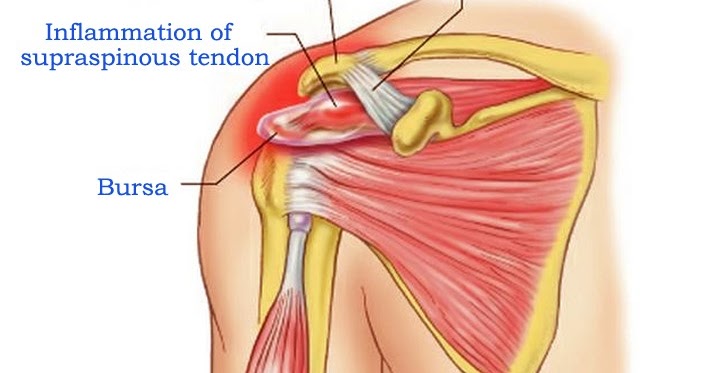
The above conditions often respond very well to physiotherapy treatment which includes manual therapy, dry needling, extracorporeal shockwave therapy, exercise programs involving stretching, strengthening the rotator cuff and stabilising the scapula (shoulder blades). Supraspinatus tendinopathy or supraspinatus "tendinitis" is a common source of reported shoulder pain in patients that perform repetitive overhead activities, overloading the tendon. Examples of this include painting, hairdressing or sports requiring overhead actions such as tennis and volleyball. This is commonly clinically diagnosed by experienced physiotherapists and formally confirmed on shoulder ultrasound scans. The supraspinatus tendon is part of the rotator cuff muscle group in the shoulder, involved in stabilising, "externally rotating" and "abducting" the shoulder (side raise). The tendon often experiences impingement as it passes in between the humeral head ("ball and socket" joint) and acromion (the bony process on the shoulder blade). Friction between the tendon and acromion is reduced by the subacromial bursa which can also get inflamed causing "subacromial bursitis".
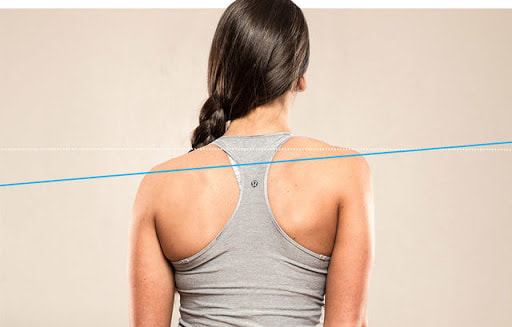
Supraspinatus tendinopathy can cause significant reduced shoulder function, pain, strength and range of motion, particularly with overhead activites. Physiotherapy treatment is often the first line of treatment before a cortisone injection is considered. Manual therapy, extracorporeal shockwave therapy, dry needling and a rotator cuff strengthening and shoulder stabilisation exercise program often can help resolve the problem quickly. "Uneven shoulders" are often noticed when you look in the mirror as you get dressed after a shower. This can be a cause of various symptoms such as tension headaches, pain, tightness, pins and needles and a lack of general mobility in the neck and shoulders. Most of the time, it is not a major health concern. Common causes include:
If you are worried about having "uneven shoulders", please do not hesitate to get it professionally assessed by an appropriately trained physiotherapist or your GP. |
Author
Archives
May 2024
|
Copyright Acland Street Physiotherapy © 2024


 RSS Feed
RSS Feed